
Signs of Stomach Ulcers
Stomach ulcers are open sores that develop on the lining of the stomach or small intestine, but heartburn is caused when stomach acid flows back into the esophagus.

Traveling with Celiac disease can be a daunting experience. From navigating unfamiliar menus to worrying about cross-contamination, leaving your safe gluten-free bubble may seem overwhelming.
But fear not! With these helpful tips, you can still enjoy delicious meals and stress-free travel while maintaining your gluten-free diet.
Before you pack your bags, take the time to research gluten-free dining options at your destination. Look for restaurants that offer certified gluten-free foods or have a strong reputation among the gluten-free community. Many places now boast online menus or utilize apps dedicated to helping those with dietary restrictions.
Bookmarking these resources or using social media to contact local celiac disease support groups can also provide information and personal dining recommendations. Preparing a list of safe dining spots can help alleviate the stress of finding gluten-free options on the fly, ensuring a more enjoyable and worry-free travel experience. When you arrive, plan a trip to a local grocery store and pick up some of your favorite snacks.
Navigating gluten-free dining in larger cities can often be a smoother experience for those with celiac disease. Metropolitan areas tend to have a wider variety of restaurants and eateries knowledgeable about celiac disease and better equipped to cater to gluten-free diets. This is partly because big cities usually have a more diverse population, including those who require or prefer a gluten-free diet for health reasons.
Consequently, you’re more likely to find dedicated gluten-free bakeries, cafes, and even pizza places. Additionally, larger urban centers tend to be more familiar with handling dietary restrictions and preventing cross-contamination, giving you a broader spectrum of worry-free dining options.
A stash of gluten-free snacks on hand can be a lifesaver during your travels, especially when gluten-free options are scarce or when you’re moving. Pack nutritious and satisfying snacks like gluten-free granola bars, nuts, dried fruits, or crackers. These can tide you over during long flights, road trips, or when exploring areas where gluten-free options might not be readily available.
Additionally, they can be a backup when meals get delayed, ensuring you always have a safe and convenient option at your fingertips. Preparing and packing your snacks gives you peace of mind and helps maintain your energy levels and mood, allowing you to enjoy your travels fully.
Finding gluten-free dining options can significantly enhance your travel experience, especially if you have celiac disease. Many restaurants now recognize the importance of catering to customers with specific dietary needs and offer a variety of gluten-free dishes. Look for establishments that clearly understand cross-contamination risks and take the necessary precautions to ensure your meal is safe. Some restaurants may even offer a separate gluten-free menu or mark gluten-free items clearly on their main menu.
Additionally, international cuisines such as Mexican, Thai, and Indian often have naturally gluten-free dishes due to their reliance on rice and corn as staple ingredients. Don’t hesitate to communicate your dietary restrictions to your server or the restaurant’s chef. They can guide you to finding the safest and most delicious options, ensuring you can confidently dine and enjoy your meal without worrying.
When dining out, individuals with celiac disease must ask the right questions to ensure their meal is safely prepared without any risk of gluten contamination. Tell your server about your dietary restrictions and inquire whether the restaurant is accustomed to handling gluten-free requests. Ask about specific menu items and how they are prepared, including whether a kitchen has a dedicated gluten-free area.
It’s essential to verify if common items like fryers and cutting boards are shared with gluten-containing foods, which could pose a risk of cross-contamination. Questions regarding ingredients in sauces, dressings, and marinades can also help avoid hidden sources of gluten. Clear and open communication with the restaurant staff educates them about your needs and significantly increases the likelihood of a safe and enjoyable dining experience.
If you are experiencing symptoms that could indicate celiac disease, such as chronic gastrointestinal issues, unexplained weight loss, persistent fatigue, or nutrient deficiencies, it’s critical to consult with your healthcare provider. Celiac disease can manifest in various ways and impact multiple body systems beyond the digestive tract, including dermatological, reproductive, and neurological effects.
Do not attempt to self-diagnose or start a gluten-free diet without professional guidance, as this can interfere with the accuracy of celiac disease tests. A proper diagnosis typically involves blood tests followed by an endoscopy to assess damage to the small intestine. If you have a family history of celiac disease, it’s also advisable to speak with your doctor, as genetics play a significant role in the development of this autoimmune disorder.
Your healthcare provider can help you navigate dietary changes and provide resources for managing gluten-free travel. So, don’t wait to seek medical advice if you’re experiencing symptoms or suspect that you have celiac disease.
Gluten-free traveling is challenging, but we hope you will be well prepared. If you need further help, please contact Allied Digestive Health. Let’s work together to keep you happy and healthy.

Stomach ulcers are open sores that develop on the lining of the stomach or small intestine, but heartburn is caused when stomach acid flows back into the esophagus.

Poorly absorbed carbs may ferment in the gut, leading to symptoms such as bloating, gas, diarrhea, or constipation.

If left untreated, GERD can lead to complications including esophagitis (inflammation of the esophagus), strictures (narrowing of the esophagus), or even Barrett’s esophagus, a condition that increases the risk of esophageal cancer.

IBS-C often requires a tailored approach that incorporates dietary changes, stress management, and sometimes prescribed medications to regulate bowel movements and reduce discomfort.
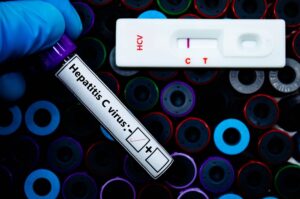
Hepatitis C can affect women differently due to hormonal variations, immune system responses, and unique physiological factors

This connection means that stress, anxiety, and other psychological factors can directly impact gut function, leading to symptoms like abdominal pain, bloating, and irregular bowel movements.

Chronic inflammation associated with IBD can lead to complications such as joint pain, skin conditions, eye issues, and more.

How different types of fiber affect IBS is crucial to creating a diet that supports digestive health without triggering flare-ups.

Lactose Intolerance occurs due to a deficiency of lactase, the enzyme responsible for digesting lactose in the small intestine.

This condition can result from various factors, including poor diet, stress, infections, or underlying health conditions like IBD.

One of the most essential steps in managing IBS is identifying specific triggers and paying attention to your body’s unique responses.

Although the symptoms of IBS can vary widely from person to person, several common signs are associated with the condition.
For Your Visit
Brick Office
P: 732-458-8300
Brick Medical Arts Building
1640 Route 88, Suite 202
Brick, New Jersey 08724
Mon – Fri: 8:30AM – 5:00PM
Sat & Sun: Closed
Neptune Office
P: 732-776-9300
Jersey Shore Medical Arts Building
1944 Corlies Ave. Suite 205
Neptune, New Jersey 07753
Mon – Fri: 8:30AM – 5:00PM
Sat & Sun: Closed
Jackson Office
P: 732-928-2300
706 Bennetts Mills Road
Jackson, New Jersey 08527
Mon – Fri: 8:30AM – 5:00PM
Sat & Sun: Closed
© All Rights Reserved